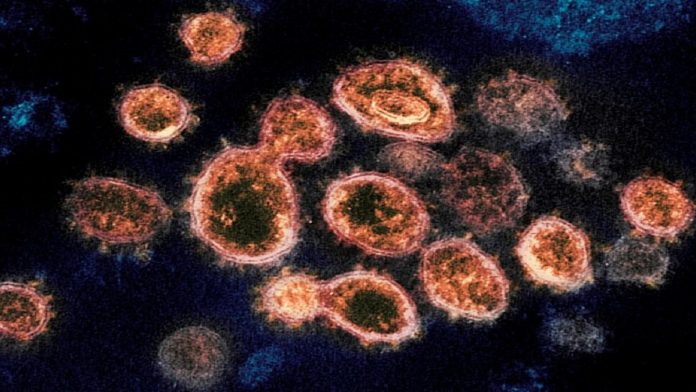
Drug Maker Pfizer says a new covid-19 pill that has been developing cuts the risk of hospital admissions or death by nearly 90 percent a trial of the experimental drive was even stopped early.
Pfizer Inc. announced Friday that its experimental COVID-19 antiviral pill reduced hospitalization and death rates in high-risk people by nearly 90%, joining the race for an easy-to-use coronavirus treatment.
The majority of COVID-19 therapies now require an IV or injection. After demonstrating promising early results, competitor Merck’s COVID-19 tablet is already under evaluation by the Food and Drug Administration, and the United Kingdom became the first country to approve it on Thursday.
After independent experts suggested halting the company’s trial due to the strength of its results, Pfizer said it will approach the FDA and international regulators to approve the drug as soon as feasible. The FDA might reach a decision in weeks or months after Pfizer submits its application.
Researchers have been rushing to find a tablet to treat COVID-19 that can be used at home to relieve symptoms, expedite recovery, and keep people out of the hospital since the pandemic began last year.
Having pills to treat early COVID-19 “would be a very important advance,” said Dr. John Mellors, chief of infectious diseases at the University of Pittsburgh, who was not involved in the Pfizer study.
“We could phone in a prescription to the local pharmacy if someone showed symptoms and tested positive, like we do for many, many infectious diseases,” he said.
Pfizer revealed preliminary findings from a 775-adult trial on Friday. When compared to patients who took a placebo pill, individuals who received the company’s medicine paired with another antiviral quickly after developing COVID-19 symptoms had an 89 percent lower combined rate of hospitalization or death after a month.
Only around 1% of people who took the medicine needed to be admitted to the hospital, and no one died. In the comparison group, 7% of people were admitted to the hospital, and seven people died.
In an interview, Dr. Mikael Dolsten, Pfizer’s chief scientific officer, stated, “We were expecting for something remarkable, but it’s uncommon that fantastic treatments come through with almost 90% efficacy and 100% protection against mortality.”
Participants in the study were unvaccinated, had mild-to-moderate COVID-19, and were at high risk of being admitted to the hospital due to health issues such as obesity, diabetes, or heart disease. Treatment started three to five days after the onset of symptoms and lasted five days. Patients who received the medicine sooner had somewhat better outcomes, emphasizing the need of prompt assessment and treatment.
Pfizer provided few details on side effects, but said that the rates of problems were about 20% in both groups.
When intermediate findings reveal such an obvious benefit, an independent group of medical professionals overseeing the trial suggested discontinuing it early, as is customary protocol. The data has not yet been made public for outside assessment, as is customary when new medical research is being evaluated.
Vaccination, according to top US health officials, will continue to be the greatest approach to guard against infection. However, with tens of millions of adults worldwide remaining unvaccinated, effective, easy-to-use therapies will be vital in preventing future outbreaks
The FDA has scheduled a public meeting for later this month to discuss Merck’s molnupiravir tablet. In September, the business announced that their medicine reduced hospitalization and death rates by 50%. Because of disparities in the research, including where they were done and what types of mutations were circulating, experts warned against comparing preliminary results.
“It’s too early to declare a winner in the 100-meter dash,” Mellors remarked. “There’s a substantial difference between 50% and 90%, but we need to make sure the populations are equivalent,” says the researcher.
Although Merck’s tablet is further along in the regulatory process in the United States, Pfizer’s medicine could benefit from a more familiar safety profile with fewer red flags for regulators. Pregnant women were not allowed to participate in the Merck trial due to the danger of birth abnormalities, whereas Pfizer’s medication had no such limits. The Merck medicine disrupts the coronavirus by interfering with its genetic coding, which is a novel approach to virus disruption.
fizer’s medication is a protease inhibitor, a class of antiviral agents that has changed HIV and hepatitis C treatment for decades. The medications prevent viruses from multiplying in the human body by inhibiting a critical enzyme.
During the SARS pandemic in Asia in 2003, the drug was discovered for the first time. Given the similarities between the two coronaviruses, business researchers decided to revive the medicine and test it for COVID-19 last year.
The United States has approved remdesivir, a new antiviral medicine for COVID-19, as well as three antibody therapy to help the immune system combat the virus. However, they must be administered by IV or injection in hospitals or clinics, and limited supplies were stressed by the delta variant’s recent increase.